Hip Dysplasia
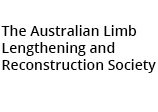
Developmental dysplasia (dislocation) of the hip (DDH) is an abnormal formation of the hip joint in which the ball on top of the thighbone (femur) is not held firmly in the socket. In some instances, the ligaments of the hip joint may be loose and stretched.
The degree of hip looseness, or instability, varies in DDH. In some children, the thighbone is simply loose in the socket at birth. In other children, the bone is completely out of the socket. In still other children, the looseness worsens as the child grows and becomes more active.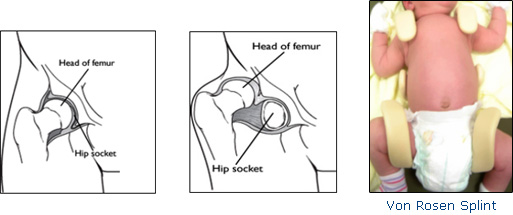
Pediatricians screen for DDH at a newborn's first examination and at every well-baby checkup thereafter. When the condition is detected at birth, it can usually be corrected. But if the hip is not dislocated at birth, the condition may not be noticed until the child begins walking. At this time, treatment is more complicated and the outcome less uncertain.
Left untreated, DDH can lead to pain and osteoarthritis by early adulthood. It may produce a difference in leg length or a "duck-like" gait and decreased agility. If treated successfully (and the earlier the better), children regain normal hip joint function. However, even with appropriate treatment, especially in children 2 years or older, hip deformity and osteoarthritis may develop later in life.
Cause
DDH tends to run in families. It can be present in either hip and in any individual. It usually affects the left hip and is predominant in girls, first born children, and babies born in the breech position (especially with feet up by the shoulders).
Symptoms
This is not a painful condition. Some babies born with a dislocated hip will show no outward signs.
Contact a pediatrician if your baby has legs of different lengths, uneven skin folds on the thigh; less mobility or flexibility on one side; or limping, toe walking, or a waddling, duck-like gait.
Doctor Examination
In addition to visual clues, the doctor will use careful physical examination tests to check for DDH, such as listening and feeling for "clunks" as the hip is manipulated. For older infants and children, X-rays of the hip may be taken. Occasionally, an ultrasound scan soon after birth may assist with the diagnosis.
Nonsurgical Treatment
Treatment methods depend on the child's age.
Newborns
Newborns are placed in a Von Rosen Splint for 6-8 weeks, to treat DDH. This splint keeps the thighbone in the socket. This will help tighten the ligaments around the hip joint and promote normal hip socket formation.
1 to 6 months
The baby's thighbone is repositioned in the socket using a harness or similar device. The method is usually successful. But if it is not, the doctor may have to anesthetize the baby and move the thighbone into proper position, and then put the baby into a body cast (spica).
Surgical Treatment
6 months to 2 years
The child is placed under anesthesia, and the thigh bone is manipulated into the proper position in the socket. Open surgery is sometimes necessary. Afterwards, the child is placed into a body cast (spica) to maintain the hip position.
Older than 2 years
Deformities may worsen, making open surgery necessary to realign the hip. Afterwards, the child is placed into a body cast (spica) to maintain the hip in the socket.
In many children with DDH, a body cast and/or brace is required to keep the hip bone in the joint during healing. X-rays and other regular follow-up monitoring are needed after DDH treatment until the child's growth is complete.
The Von Rosen Splint
The splint is not removed during the treatment phase. The baby is bathed in the splint.
Drying where the splint contacts the baby's skin is imperative to avoid skin rash. Try to avoid skin lotions or powders. These seem to irritate the skin under the splint.
You should vary the baby's position by propping her/him with a rolled towel, so that time is spent in other than the "flat on back" position. This will help avoid "flattening of the back of head" or plagiocephaly.
Sometimes during changing/feeding or burping, the baby's shoulders will come forward – out of the splint. This is NOT a problem, and baby should be repositioned to allow him/her to fall back into the splint.
In most cases, an appointment approximately one week from the splint application will need to be made by yourselves. At this appointment, Dr Astori will check the splint and make arrangements for future follow up including USS.